Part of Action from learning report 2022/23
Action for learning in 2023-23: changing how we work
Integrated care systems (ICSs) in action
Making change happen in Birmingham and Solihull
Birmingham and Solihull ICS (BSOL) in partnership with commissioners, experts with a learning disability and autistic people, self-advocacy groups and other stakeholders, launched a three-year public facing strategy for LeDeR in 2022. This aims to improve the experiences in health services for people with a learning disability and autistic people.
The strategy embeds learning from LeDeR into all aspects of the local system and is based on over 500 recommendations from more than 200 local LeDeR reviews. It comprises 20 priority areas for change which all the partners identified together.
Improvements to coordinated care have already been made against these priorities
[19]
by strategy partners including:
- Midland Mencap after an audit at University Hospitals Birmingham discovered that only 15 of the 300 people with a learning disability or autistic people who were hospitalised in Birmingham in 2022 had a hospital passport, prioritised producing these. The passports share a person’s likes and dislikes with staff– helping to break down barriers in communication. They have helped produce more than 100 passports so far.
- Health and social care commissioners at Birmingham City Council helped to share the learning from the success of the hospital passports scheme and encouraged over 1000 providers (e.g., care homes) to ensure their residents have them.
Commissioners –also changed their approach to monitoring providers, embedding LeDeR learning in their monitoring and quality assurance – for example by providing training and examples to providers of what good quality care should look like. They can also penalise a provider through contractual action if it doesn’t meet these standards.
The BSOL LeDeR team share knowledge across social work teams, so that annual health and social care reviews fully consider all aspects of a person's wellbeing, and they work strategically with social care colleagues and with providers to embed LeDeR. The team can raise any issues to the commissioners which informs the quality monitoring of providers with urgent action where needed, giving a provider a timeframe to respond with any necessary actions required.
Reinforcing the strategy is conducted through:
- Formal governance groups and regular meetings including a monthly LeDeR review oversight panel with representatives from the council, Mencap, self-advocacy services, primary care, acute care, specialist learning disability teams and others who openly discuss the changes they can feed into their organisations.
- The Action Learning Group in BSOL which is also reinforcing the 20 priorities through training in GP practices, at day centres and at specific events. The strategy group are asking everyone involved if it is working and, as a result, and strategy partners are feeling more empowered to advocate for their members and call for changes, based on the 20 priorities and a clear understanding of the standards that everyone should expect.
Capturing change:
BSOL LeDeR has funded a ‘capturing change’ project, contracting Solihull Action through Advocacy, Midland Mencap and Experts by Experience Solihull CIC to work together over the next 3 years to listen to feedback on how the strategy is working from people with lived experience, families, carers and individuals.
Improving standards across all NHS services within priority groups
People with a learning disability and autistic people have been more formally recognised as priority groups across all areas of the NHS in recent years. Learning from LeDeR is enabling us to embed these priority groups in all our services for individuals. In 2022/23 we worked strategically to improve standards in our systems, emphasising people with a learning disability and autistic people at the heart of our work. These include improvements in the following four areas:
- Benchmarking NHS Trusts
In 2018 NHS England published four learning disability improvement standards to help NHS Trusts improve the quality of care they provide people with a learning disability and autistic people. These were co-produced by people with a learning disability and families and are based on respecting and protecting rights, inclusion and engagement, the workforce, and specialist services.
To support Trusts to make improvements NHS England commissioned an annual national benchmarking programme which involves asking NHS staff, people who use NHS services and families/carers about how services are doing, so they can identify what they do well and where they need to do better.
In 2022/23 we added questions to specifically ask Trusts how learning from LeDeR has been applied in the organisation and what service improvements have been made as a result.
The findings are published on the NHS Benchmarking Network and in 2021 to 2022 showed: People accessing trusts with a learning disability liaison service reported better experiences, improvements in inclusion and engagement with people with a learning disability, autistic people and their families, NHS trusts of all types reported greater availability of learning disability and autism awareness training, and there are more staff providing specialist services in trusts and in the community.
- Core20PLUS5
People with a learning disability and autistic people are now specifically included as priority groups in Core20PLUS5 – a new NHS England approach to reducing healthcare inequalities.
Core20PLUS5 defines a target population – the ‘Core20’ – that is, the most deprived 20% of the national population identified by the national Index of Multiple Deprivation (IMD), plus specific population groups including minority ethnic groups, inclusion health groups, and now ‘people with a learning disability and people who are autistic’. The ‘5’ in refers to the five clinical areas of focus for accelerated improvement including severe mental illness, early cancer diagnosis, and respiratory diseases. ICBs must ensure that people with a learning disability and autistic people are considered when tackling local health inequalities.
- Learning disability, autism and NHS operational priorities for 2023/24
NHS operational planning and contracting guidance for ICBs for 2023/24 gives details of the health priorities for the year ahead. The guidance reconfirms the ongoing need to recover core NHS services and improve productivity, making progress in delivering the key NHS Long Term Plan ambitions and continuing to transform the NHS for the future.
The specific objectives to improve services for people with a learning disability and autistic people are to:
- ensure 75% of people aged over 14 on GP learning disability registers receive an annual health check and health action plan by March 2024
- reduce reliance on inpatient mental health care, (while also improving the quality of inpatient care) so that by March 2024 fewer adults and children with a learning disability and autistic people are cared for in an inpatient unit
- continue to prevent and address health inequalities and deliver on the Core20PLUS5
- The NHS Standard Contract for 2023/24
There is an increased focus on people with a learning disability and autistic people in the new NHS Standard Contract which runs from 1 April 2023 to 31 March 2024. This contract is used when any NHS service is commissioned (except primary care). Some of the additions to the contract were based on recommendations from the LeDeR team and include:
- guidance on end of life care now also including the Universal Principles for Advance Care Planning (Published in March 2022) and guidance on DNACPR
- the requirement for providers to report the death of people with a learning disability and autistic people who died while they were known to their services using the LeDeR platform.
Annual health checks (AHCs)
An Annual Health Check (AHC) is a regular opportunity to promote a healthy lifestyle, support wellbeing, and enable early access to additional healthcare support if an individual needs this. It is important that everyone over the age of 14 who is on their doctor's learning disability register has an AHC as it can also help spot the early signs of illnesses such as cancer and diabetes, or respiratory and heart issues. This can lead to earlier treatment and better health outcomes.
An AHC is also an opportunity to discuss vaccinations, screening, manage and monitor known health conditions such as epilepsy or dysphagia (swallowing difficulties), and to discuss Do Not Attempt Cardiopulmonary Resuscitation decisions. A doctor, pharmacist, nurse or healthcare assistant can conduct an AHC, with final oversight from the GP. Every AHC should be supported by a health action plan (HAP) for the individual.
In our work to drive the uptake and quality of AHCs in 2022/23 we:
Led events, webinars or gave presentations:
- about the importance of and best practice in AHCs and about the learning disability register for GPs. We also established a community of practice to share good practice including how AHCs can be delivered by different practice staff to reduce demands on GPs. Over 800 people attended and events continue to run throughout 2023. The guidance on best practice in AHCs is available on the FutureNHS platform (For NHS staff).
- on the importance of AHCs in reducing health inequalities for people with a learning disability and autistic people to Academic Health Science Networks ( AHSNs), provider forums, regional health inequality meetings and at BILD’s GOLD conference on ageing well
Produced new resources and reports including:
- a film portraying Charlotte’s AHC and Health Action Plan (HAP) which is easily accessible and can be used as both a training resource and to help people understand what a good quality AHC should look like
- a report from the National Autistic Society who we commissioned to engage harder to reach groups – including homeless people, transgender people – and ask how to support them with AHCs.
- a new document for parents/carers (including a plain English and easy read versions) to support conversations with GPs about adding children and young people to the register as part of a primary care review on the quality and improvement of AHCs and the register. (To be published in late 2023)
Worked nationally and regionally to:
- include AHCs in local health policies where appropriate and to update aspects of 2023/24 contracts to ensure AHCs are included –for example in the NHS Standard Contract for people in inpatient settings, and the Specialist Commissioning Service Specification to include AHCs for those in private hospitals. The primary care contract continues to include AHCs - with a greater emphasis on ethnicity recording and HAPs
support several regional exemplar sites working to improve access to and uptake of AHCs.
Autism specific annual health checks
The NHS Long Term Plan said that by March 2024 at least 75% of people aged 14 and over on a GP learning disability register should receive an AHC. However, 70% of autistic people [20] do not have a learning disability, autistic people are more likely to experience poor health [21] , and the mortality rate is 1.3 times higher in autistic people than the general population[22]. Some health services and professionals could do more to provide autistic people with sufficiently adapted and supportive care.
A new pilot
The NHS long term plan also said that NHS England will, ‘pilot the introduction of a specific health check for autistic people, and if successful, extend it more widely’. We have now funded four NHS regions to deliver this pilot - the East of England, North East and Yorkshire, London, and the Midlands. Primary care practices in these areas delivered their first health checks for autistic people in January 2023 and are conducting around 480 autism specific health checks this year.
Every stage of the process is providing information on the practicalities of both offering and implementing specific checks for autistic people e.g. about how GP practices can accurately identify all their autistic patients A full evaluation will collate all the learning and identify any themes that have arisen.
A randomised controlled trial (RCT)
Although the process and ethos of the health checks for autistic people is similar to those for people with a learning disability, the autism specific health check is based on a template co-produced by Newcastle University who were commissioned by NHS England and Autistica to develop it.
The University was also commissioned to test for clinical outcomes for autistic people as part of a randomised controlled trial (RCT). An RCT typically compares a new treatment with an existing standard of care and in this case to identify previously unmet clinical needs. The bespoke template includes holistic questions around medication, mental and physical health problems, eating and sleeping. It aims to reinforce the importance of considering an autistic person’s sensory needs, for example around reducing noise or limiting touch, raise awareness of the need for reasonable adjustments and ultimately improve access to mainstream healthcare. The RCT will report in 2024.
In Brief - other annual health check improvements
The North West
Greater Manchester ICP worked with Manchester People First - a self-advocacy group for adults with a learning disability and AJs Academy - an activity resource day centre which supports individuals who have a learning disability and their families, to co-produce easy read documents to support the AHC Process. They also co-produced a ‘patient journey map’ which will be used to develop quality measures for AHCs in 2023/24 to deliver a clear, consistent approach to AHCs.
North East and Yorkshire
NHS England funded pilot approaches in annual health checks. One of these resulted in the Bridlington Learning Disability and Wellbeing Hub, which opened in late 2022 is based in the Bridlington Primary Care Network. The community learning disability team have created a series of videos around AHCs, describing their holistic approach to wellbeing through social prescribing. Other PCNs in their ICB are now looking to use this model.
South Yorkshire ICB (Sheffield Place) asked all their GP practices to prioritise AHCs for people who did not receive a check in 2021/22. They also commissioned an outreach initiative led by Sheffield Mencap and Gateway (SMG) where SMG supported hard to reach patients to attend their AHC. Several surgeries were also involved in a pilot led by Foundry Primary Care Network to use Care Coordinators and Physician Associate roles in GP practices to conduct AHCs. As a result of these and other efforts, 3,382 health checks were recorded in Sheffield in 2022/23 - meaning 889 more people [23] received an AHC than in the previous year.
As a very busy practice we don't always have the time or resources to try and reach out, but with your help we've been able to engage with more patients and ensure they have a yearly health check. Many of our patients have benefited from your support by accompanying them to appointments they otherwise may not attend or [by your] offering advice and guidance. Your help has been invaluable to our practice and our patients."
An updated toolkit for London
The AHC Toolkit for London, a comprehensive guide for GPs to support the completion of good quality AHCs, which was first published in late 2021, has been reviewed, refreshed, and republished. It is now available on the FutureNHS site (for NHS staff) and has been circulated to GPs and PCNs across London.
Children and young people in the Midlands
The Midlands Learning Disability, Autism and SEND Team have worked together with partners across the Midlands to improve the uptake and experience of AHCs among children and young people aged 14 and over with a learning disability. LeDeR reviews show take up of AHCs is lower in younger people.
A new Midlands Regional AHC Improvement Framework has been developed using intelligence from events attended by health and social care partners. It outlines a series of five priorities and goals, the actions required to achieve them, and examples of good practice in AHCs for children and young people. One action will embed AHCs into the education, health and care plan (EHCP) process while another suggests local authorities and health commissioners work together to ensure a smooth transition for young people to adult services.
The framework has been circulated widely across all systems, GP practices, SEND boards and learning disability and autism networks in the Midlands - and the region is already seeing improvements. By December 2022, over 500 more AHCs were completed for children and young people compared to Dec 2021.
Race, Religion, Ethnicity and Culture
LeDeR reports show that people from a minority ethnic group with a learning disability have even poorer outcomes than other people with a learning disability.
In response NHS England has commissioned a series of projects we are either leading or supporting. These include:
- improving ethnicity recording
- tackling health inequalities
- focused LeDeR reviews
- anti-racism initiatives
- intersectionality training.
Recording ethnicity
We worked to amend the (Investment and Impact Fund) IIF indicator for learning disability in AHCs to include a requirement to record ethnicity for people with a learning disability. This has now been included from April 2023 and outlined in the new GP contract letter which was published in March 2023.
Tackling the barriers that drive health inequality
We commissioned work from the NHS Race and Health Observatory to help us to better understand the reasons behind health inequalities faced by people with a learning disability who are from a minority ethnic background and to suggest practical solutions to these barriers that the NHS and our partners could take.
Their report, ‘ We deserve better: Ethnic minorities with a learning disability and access to healthcare’ published in July 2023 and went to the July meeting of the NHS England Board, was produced with the University of Central Lancashire (UCLan), partner organisations, and a working group of people with lived experience. It makes a number of recommendations at ICB, regional and national level, as well as making recommendations for those commissioning and conducting research around health and care. The main recommendations include:
- the development of future health and social care policies should, as standard, include advice emphasising coproduction approaches to tackling health inequalities experienced by people with a learning disability from ethnic minority backgrounds
- improving the completeness and accuracy of ethnicity coding of people with a learning disability across all NHS and care providers
- LeDeR reviewers should ensure that they accurately record in the LeDeR review the ethnicity of the person whose death they are reviewing
- specific research in under-represented groups such as asylum seekers, the Jewish community and Irish Travellers should be commissioned
NHS England is working with partners to develop an action plan to address the recommendations which will go to a meeting of the NHS England board in Autumn 2023. The work will build on the requirement introduced 2023 for GPs to record ethnicity as part of the learning disability annual health check.
Focused LeDeR reviews
A ‘focused’ LeDeR review is conducted into the death of every person with a learning disability from a minority ethnic group notified the system. Once a death is reported to LeDeR a reviewer conducts an ‘initial’ LeDeR review by talking to family, carers and professionals involved in the person’s care. A focused review looks in more detail at the person’s life.
ICBs use this evidence to drive service improvements in health and social care for people from minority ethnic groups in their area. In addition, every ICB has a named lead for minority ethnic groups on their LeDeR governance group.
Intersectionality training
NHS England has also delivered a ‘train the trainer’ programme to support LeDeR reviewers and local systems to consider ‘intersectionality’ – that is how the different aspects of someone’s identity, for example race, culture and religion, can overlap or ‘intersect’ with their learning disability or autism and significantly increase health inequalities in the quality of care and support provided to the person during their life.
More than 130 people from ICBs across England were trained by January 2023 as LeDeR intersectionality trainers which will enable them to cascade their knowledge across local systems so that their local workforce is trained. This will equip staff to consider issues of intersectionality as an essential part of reviews.
The training includes three films on intersectionality which feature conversations with people with a learning disability and autism and their families. Exploring issues of culture, race, ethnicity, religion and experience of care, the films have been shared extensively across all mental health trusts in the Mental Health Learning Disability bulletin and across Learning Disability staff.
Feedback from the delegates who attended the intersectionality training so far has been extremely positive:
It really made me think about power and inequality and how I can ask questions in a curious and respectful way.”



The ‘Equal Treatment’ Project
An anti-racism initiative funded by NHS England and led by Learning Disability England (LDE), saw seminars, workshops and training delivered throughout 2022. The Equal Treatment project challenges racism and health inequalities through strengthening self-advocacy and peer support. LDE worked in partnership with the charities Changing Our Lives, Contact, and IncludeMeToo.
The project aims to:
- strengthen self-advocacy and parent/carer organisations’ work with people with a learning disability from minority ethnic groups and their families
- increase the confidence of local organisations led by people from minorityethnic groups in working with people with a learning disability and their families when tackling health inequalities
- link these efforts with wider initiatives to reduce premature mortality and health inequalities.
So far, three distinct strands of work have been delivered in these areas including:
Strand 1
Changing Our Lives, which aims to reframe how society views mental health and disability, delivered training to 10 organisations which included three sessions in person with 38 self-advocates and online training workshops for 20 senior staff from the 10 organisations. Several resources including short films, images and resource explainers were developed as part of this work.
Strand 2
Contact, for families with disabled children, co-developed and delivered a three workshop training programme for 13 parent/carer forums based on the participating organisations’ needs. The training covered understanding representation and inclusion, intersectional disadvantage, identification of information gaps and action planning.
Strand 3
Seminars run by IncludeMeToo, a charity for children and young people with a disability and their families, aimed to raise awareness among wider community organisations of the racism and inequalities that could be faced by people with a learning disability from minority ethnic groups. Their seminars shared knowledge, challenged assumptions, and planned actions to tackle inequalities.
Finally, LDE hosted a sharing session in September 2022 which was attended by more than 50 delegates. All three work strands shared their key learning from their projects. The recording of the session is available here.
Feedback from this session demonstrated an appetite to continue the discussions, training and ultimate work in this area.
Leadership training for people with a learning disability and autistic people
NHS England has funded a project and survey from Learning Disability England which will help us and our partners to assess what leadership training opportunities there are for people with a learning disability and autistic people, who are from a minority ethnic group. We also want to identify and understand how the experiences of ethnic minority people, intersectionality, anti-racism, and inclusive practice are included in these programmes.
When LDE worked with people and organisations as part of the Equal Treatment and Working Together to get the job done projects they heard from some people that leadership training does not always include people from minority ethnic groups with a learning disability or autistic people. They also learnt that training about different people’s experiences and anti-racism practice is not always accessible.
The LDE survey which was completed in spring 2023 asked what leadership or similar training there is aimed at or led by people with a learning disability or autistic people. The results from the survey and project will help us to understand current training opportunities and will see the production of an accessible report summarising improvement ideas.
Improving access to health in minority ethnic groups
In 2022 NHS Bristol, North Somerset and South Gloucestershire (BNSSG) ICB commissioned Autism Independence to explore the lived experiences of accessing health services among black and other minority ethnic groups where there is a young person aged over 16 in the family who is autistic or has a learning disability.
The charity worked with 42 families before presenting their findings in January 2023. They were joined by the families at the launch and enjoyed a celebratory meal afterwards with the Somali community. The report was also later presented at the South West’s regional Health Inequalities Improvement Group.
The report found that there was poor health engagement with AHCs, screening programmes and health appointments. The ICS is now looking to establish two ‘care navigator’ or bridging worker roles which will work with families where English is not their first language. The postholders will provide support and signpost parents and young people with a learning disability and autistic young people from minority ethnic groups to better access health services. This two-year pilot scheme will see care navigators recruited from minority ethnic groups and, if successful, it is proposed that the posts will become permanent.
BNSSG is also funding training which will be developed with community leaders to help improve access to health services among minority ethnic groups where there is an autistic person or a person with a learning disability in the family.
End of life care and advance care planning
LeDeR reviews have highlighted some issues for people with a learning disability and their families around informed choices for end of life care and decisions around any potential Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) recommendations. The 2021 LeDeR Report [24] indicates that there were still a significant percentage of cases where good practice in DNACPR decision making was not demonstrated. NHS England has co-produced a number of resources and a national framework focused on ensuring equality in access to end of life care and palliative care to tackle these inequalities for people with a learning disability [25] .
The pandemic and the Care Quality Commission (CQC) report Protect, respect, connect – decisions about living and dying well during COVID-19, reinforced that people with a learning disability must be centre stage in making their own end of life plans. NHS England and partner organisations developed Universal principles for advance care planning in March 2022 to support this, by making recommendations including the use of an ‘advance care plan’. These plans should be personalised - developed with the person and/or their family and carers - and should be sharable and clearly document what matters to the person, their preferences and decisions about future care and treatment.
NHS England also worked with NHS Digital (now part of NHS England) to develop a code on the clinical record that specifically identifies that a conversation has taken place every year with a person with a learning disability and/or their family and carers about DNACPR. This practise started in April 2022 and means that GPs are now expected to add a SNOMED CT* code to a person’s clinical record during their annual health check to confirm that a conversation has taken place about DNACPR. In future we will be able to have better confidence that a DNACPR has been put in place appropriately. *A SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms) code is a shared language used in electronic health records enabling information to be shared more easily between them.
In March 2023 we sent a letter to clinical leads and chief nurses in ICBs, medical directors and executive directors of nursing in NHS Foundation Trusts, and all GPs and primary care nurses to remind them and their systems of the importance of the appropriate use of DNACPR decisions for people with a learning disability and autistic people. This also stressed the importance of implementing the Universal principles for advanced care planning and ensuring that DNACPR decisions for people with a learning disability and autistic people are appropriate, are made on an individual basis and that conversations are reasonably adjusted.
Regional projects to improve future planning
Many self-advocacy groups working with people with a learning disability are also encouraging their members to have good quality conversations about their death, while they are well, so they are better informed and can feel confident that their wishes will be considered and that they will have a greater sense of control over their ability to live and die well.
NHS England has funded three self-advocacy groups - People First Merseyside, Inclusion North and SpeakUp - to create distinct projects in advance care planning which will strengthen our efforts in this area. The projects will be delivered by the end of 2023 and will create a collection of easy read materials, workshop plans, bespoke training, and films. These resources and any learning from developing them will be cascaded by NHS England and our partners.
Informing choices on DNACPR in the North West
People First Merseyside are using their funding from NHS England to create national resources to empower people with a learning disability and their families to make informed choices around DNACPR in any future end of life care.
This initiative will build on the success of their Dignity and Voices in Dying project ‘ DAVID’ which was named in honour of a service member who sadly died. David had no family and the group realised they did not know what his final wishes were so People First’s members decided to do some work around planning for their own end of life choices, and the DAVID project was created.
DAVID aims to bring members and their families together in ‘death cafés’ - informal settings where they discuss the subject of death and are empowered to plan ahead before they face any crisis point in their health. This enables members to be proactive in informing their choices around making a living will, power of attorney, organ donation and even the music they want at their funeral.
Members are also working with ‘Task and Finish’ groups to:
- create a resource pack for will writing with information for both people with a learning disability and families/carers
- collate materials for an ‘organ donation resource pack’ they are producing
- try out activities for potential inclusion in the above packs and seek feedback at the cafés.
The DNACPR work will see the team and People First members behind the DAVID initiative create a new film, produce a resource booklet, and deliver awareness raising sessions across the North West on DNACPR issues. The DNACPR work will be delivered later in 2023 and the resources made widely available.
End of life conversations in death cafés
Inclusion North has used the NHS England funding to support improvements in end of life conversations among people with a learning disability, autistic people and their families and by:
- raising awareness of good practice with health professionals across the North East, Yorkshire and Humber
- developing resources to support people with a learning disability, autistic people and their families to get more comfortable talking about death, dying and making plans for the future.
They are working with their Stop People Dying Too Young Group and local palliative care professionals to ensure that experts lead this work.
To support people with a learning disability, autistic people and their families to get more comfortable talking about death, dying and making plans for the future they are creating resources which will be cascaded to support others to run facilitated conversations at ‘ death cafés’.
Although the name ‘death cafés’ may seem unpalatable, the group feel that it reflects the need for the language around death and dying to be straightforward - by using the words ‘death’ and ‘dying’ and not euphemisms which can be confusing such as saying someone is ‘lost’ or has ‘passed away.’ The sessions will include supportive guidance and tackle difficult issues in fun and gentle ways.
People with a learning disability, autistic people and family carers are also deciding the content in these café sessions – choosing the topics, as well as making a film which will discuss choices and expression of their wishes earlier in their lives.
The project will create new resources by Autumn 2023 for health professionals which will be available on their site, and will signpost to the end of life pathway and existing end of life guidance for people who have a learning disability. The ‘Stop’ group are also making a video/short film for health professionals, emphasising the individual at the heart of these discussions, as people felt that their rights were being ignored. The group want to ensure that the film reminds professionals:
- Not to assume that a person does not have the capacity to make decisions
- To talk to them
- To talk to their family
- See them as a person
- To use the Deciding Right materials – an initiative for making care decisions in advance in a shared partnership between the professional and the child, young person or adult, carer or parent
- To ensure their NHS Trust is aware of the Deciding Right materials.
The ‘Stop’ group will lead on delivering the death café materials, while campaigns like Dying Matters Week will help to raise the awareness of both the new resources and the voices of people with a learning disability and autism on end of life discussions. The resources for NHS staff will also be cascaded through internal training across the North and via NHS England networks.
Training in end of life decisions
Speakup have used the funding they received from NHS England to co-produce training and supporting materials in South Yorkshire for use with people with a learning disability, autistic people and their families. The materials will facilitate two sessions in each of the following areas: DNACPR, making difficult decisions, and advance decision making. The training started in October 2022, will be completed in late 2023 and is using the ECHO training platform which provides professional training for the care industry.
All the materials produced, including an easy read and a film about bereavement, will be made available through the Speakup website and shared via the ECHO super-hub, so anyone with access to this in England can also deliver the training. The work is being supported by South Yorkshire ICB.
Mental Capacity
The Mental Capacity Act 2005 (MCA) provides a legal framework to protect people who lack the mental capacity to make their own decisions about their care and treatment and to help them take part, as much as possible, in decisions that affect them. It also covers people who have capacity and want to make preparations for a time when they might not. Compliance with MCA is a consistent theme in LeDeR reviews.
Informed decisions on vaccination in London
In October 2022, the safeguarding and learning disability and autism teams in the London region together published two documents to support healthcare professionals in respiratory networks and the over 1,150 GP practices in the regions who undertake AHCs on their approach to decision making about flu and COVID-19 vaccines where an individual lacks capacity. The guidance reiterated that all practicable steps should be taken to support the person with a learning disability to make a decision on vaccination for themselves by helping to inform the individual in a way that works for them about:
- what the vaccine is, how it works and to understand what could happen if they choose not to have the vaccine – for example how it could prevent people from becoming seriously ill with the flu virus or COVID-19
- any potential side-effects
- the process involved in having the vaccine.
The two resources included guidance on providing information to family members and/or carers where they were responsible for any decisions, and if not, where ‘best interests’ decisions must be made. This is a decision on whether it is in the person’s best interests to have a vaccine at that particular time, based on all available information and any risks to the person themselves, other residents or staff. The resources provided links to COVID-19 vaccination guidance for healthcare workers from the UK Health Security Agency (updated in October 2022), guidance on protecting yourself from the flu, and easy read COVID guides.
They also provided information on the Mental Capacity Toolkit – a comprehensive guide to support health and care professionals by the Burdett Trust for Nursing (a charitable trust which makes grants in support of nurse-led projects).
Reasonable adjustments
Under the Equality Act 2010 organisations have a legal duty to ensure that their services are as accessible to people with a disability as they are to anyone else – by making ‘reasonable adjustments’ where these are needed.
Reasonable adjustments for someone with a learning disability or an autistic person could include longer appointments, providing easy read information or having the support of a carer. They will vary from person to person.
The introduction of the reasonable adjustment digital flag (RADF)
For optimum care to be delivered, all reasonable adjustments need to be identified, recorded, and shared across the NHS and social care. A new ‘ reasonable adjustment digital flag’ in a patient’s records will do just that. The flag will ensure staff know if a patient has a learning disability or is autistic and indicates what reasonable adjustments are needed.
The digital flag has been created on the NHS Spine. Healthcare professionals and administrative staff with the appropriate security permissions can identify, record, view, add or remove information from the flag, using the National Care Records Service (NCRS). The digital flag is currently being tested in live clinical systems and will be rolled out by 2024. It will be accompanied by an Information Standard, mandating the use of the digital flag, across all health and publicly-funded social care services, across all ages, by April 2024. The reasonable adjustment digital flag will be supported by a communications campaign, staff training and an implementation plan, recognising the significant cultural change this represents.
We have published an Information Standards Notice for the RADF under section 250 of the Health and Social Care Act 2012. This provides an overview of scope and implementation timescales, and the requirements specification.
Reasonable adjustment letters for GPs
Pathways Associates, a community interest company, worked in partnership with the learning disability team in Bury ICS to produce a letter in easy read format which GP practices can send to their patients who have a learning disability and autistic patients. The letter is based on learning from LeDeR and was created to help improve the quality of reasonable adjustments in Bury, Greater Manchester.
It provides a checklist of potential reasonable adjustments including longer appointments, large print resources, and easy read invitations. Patients or their family/carer can also add details of other reasonable adjustments which a GP practice could then put into place.
The North West Regional Forum, a self-advocacy group, also wanted to help improve the reasonable adjustments made for people with a learning disability and autistic people in the region and so teamed up with Bury People First self-advocacy group, to produce a letter that people with a learning disability can complete and give to their GP practice. Both groups felt they wanted to support their community to be more proactive in informing GPs of their needs.
Both resources have been distributed by the Learning Disability Partnership Board in Bury whose members include people with a learning disability, carers, local authority, NHS and service providers. Early adopters of the ‘ reasonable adjustments digital flag’ project have also shared the resources with other early adopters. They have all found the letters helpful and easy to roll out in their areas.
Bury Local Authority added a link to the easy read letter for GP practices in their Care Act assessment form. They have also applied learning from LeDeR and others to improve the form, increase take up of AHCs, and promote information sharing and access to health. Newly completed letters will be shared with GPs.
We want to be part of the solution and help our community know their rights.”
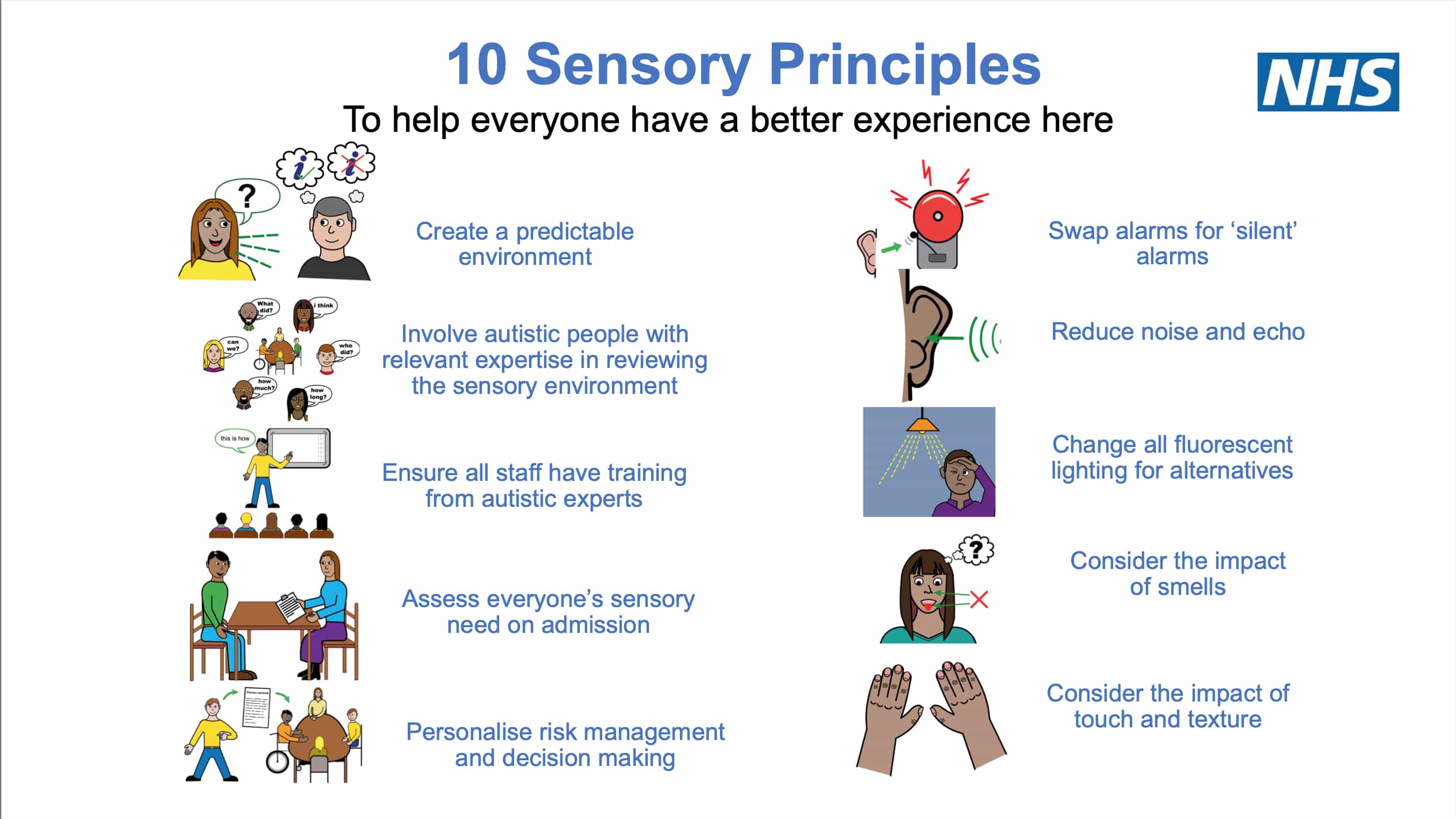
Sensory friendly resource pack
NHS England’s National Autism Team published a new sensory friendly resource pack in October 2022. The resource initially aimed to improve the environment for autistic people in mental health inpatient settings, however it can be used in any health setting, and is aimed at all health professionals working with autistic people.
Recent studies suggest sensory sensitivities are experienced by over 90% of autistic children and can persist into adulthood [26] . There are three categories of sensory sensitivities:
- hyper-sensitivity ‒ extreme over-reactivity to sensory input
- hypo-sensitivity ‒ extreme under-reactivity to sensory input
- sensory-seeking ‒ unusual interest in aspects of the sensory environment.
The pack explains how non-autism-friendly environments could impact on autistic people and hamper their recovery before providing a series of ten ward principles with suggestions on how to make a hospital ward sensory friendly. These include:
- working with autistic people to review the environment
- creating a predictable environment and reducing noise
- ensuring training is given to anyone whose role could impact on the autistic person’s experience – including cooks, cleaners, agency staff and anyone caring for the person
- considering the impact of lighting, smells, touch and texture in the personal care needs of individuals, for example, around textures such as towels
- making and regularly reviewing decisions based on an individual’s needs.
NHSE also commissioned a re-write of the Green Light Toolkit, which was first published in 2004 to help mental health services to audit and improve their service. The new version of the Toolkit (2022) has been distributed with the new sensory pack and emphasises the importance of creating accessible environments for people with sensory differences. It also has a wider choice of questions in the survey. Both resources have been shared with every ICB in England.
A new short film has been produced to describe the sensory friendly resource pack to ICSs along with a 10 sensory principles poster which lists some of the actions that local systems can adopt to help improve patients’ experience.
And Leekam SR, Nieto C, Libby SJ, et al (2007) Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37 (5), 894–910.
Making emergency departments accessible in Leeds
In 2021 the Learning Disability and Autism team at Leeds Teaching Hospitals NHS Trust conducted an audit of emergency departments. The team asked the area’s Autism Reference Group - a forum for autistic adults to have their say on services and support in Leeds - to share their experiences of the emergency department (ED). The feedback established that although some people had a positive experience, many found the ED environment stressful. For example, it could be overstimulating – increasing stress levels, leading some people to discharge themselves or reluctance among some patients to attend.
The team successfully applied for an innovations grant from the Leeds Hospitals Charity to fund the production of 350 ‘care bags’ which were designed with people with lived experience of having a learning disability or being autistic. Over 200 bags have now been distributed in the EDs in the trust since April 2022 to all patients with a known diagnosis of learning disability or autism. The bags contain items to help patients to manage in the busy waiting room in the ED, to the assessment area, during investigations and ultimately to a hospital ward if they need to be admitted.
The care bags contain:
- Easy read information about the department
- The Friends and Family Test
- Sensory and distraction items - ear defenders, an eye mask, a fidget gadget, a stress ball, an adult colouring book and pencils, and a chew ring
- An easy read evaluation form.
The Learning Disability and Autism team has trained nearly 300 staff working across all specialities in the emergency department in the use of the bags and as a result they have been made aware of 12 inpatients who needed support who they otherwise may not have been notified about. The team have also added new appropriate alerts to the records of over 50 patients and have completed new hospital passports for every appropriate patient.
The bags have proved a big hit with patients, families and staff at the hospitals – so far receiving 98% positive feedback in the ongoing evaluation.
Aaron Senior a lived experience autism advisor with NHS England received one of the bags during a visit to St James’s University Hospital and was invited to create a short film about the bags and share the work the hospital are doing. Another patient with autism who spent 10 hours in St James’s Hospital ED gave feedback to the hospital that the care bag made a huge difference when she was unwell and helped her to stay at the hospital to get the treatment she needed when she felt she may otherwise have left.
The Trust is now applying for funding to roll it out to all acute admitting areas and not just the emergency departments.
Improving urgent care in London
In April 2022 Urgent Care Plans (now called Universal Care Plans (UCP)) replaced Coordinate my Care. These electronic health records were used across London to share a person’s palliative care needs but have now been developed for use as a hospital passport for people with a learning disability and autistic people.
Staff from the Tower Hamlets Learning Disability Service contacted people with a learning disability who are known to the service and have the most complex care needs, asking them/their carer if they want an UCP and helping to complete one.
UCP forms are completed by health care professions, but future plans will enable the individual and/or their carer to complete them, with a GP or other health professional signing them off. UCPs can be accessed directly by call handlers dealing with 999 calls, the London Ambulance Service, A&E, primary and secondary care, and specialist services e.g. community learning disability services.
The plans include: a person’s significant medical history, their wishes and needs, medications, end of life choices, and any reasonable adjustments such as turn off blue lights on an ambulance if an autistic person finds them distressing.
Over 100 Tower Hamlets service users have signed up for a UCP so far and the borough aims to make the UCP become part of the annual health check process. The team have also created a short video about urgent care plans – about why they can be helpful and how to complete them – for link nurses, GPs, and others.
As the UCP template is standardised, a pan-London working group led by London Ambulance Service which includes GP leads, community and hospital learning disability liaison staff, learning disability and autism teams, and LeDeR colleagues, is now developing a more specific template for the UCP for people with a learning disability and autistic people. They have also met with two self-advocacy groups in Enfield for their views on making UCPs more accessible.
Agreement is now in place with the UCP developer, Better, and the pan-London commissioners of the UCP to take these developments forward, with a UCP template that includes specific questions about additional support needed by people with a learning disability or autism, for example, any sensory needs, soft signs of deterioration, and other conditions they may have.
Eliminating the elective care backlog for people with a learning disability
Calderdale and Huddersfield NHS Foundation Trust (CHFT) in West Yorkshire worked to prioritise patients who are more likely to experience health inequalities, including people with a learning disability and autistic people, when they tackled a backlog in elective care.
In 2021 there were 77 patients with a learning disability on a waiting list for treatment at the Trust after spikes in COVID-19 cases saw non-urgent elective treatments cancelled and staff redeployed. CHFT adopted a whole Trust approach – led by a strongly committed leadership team, to ensure priority treatment for people with a learning disability awaiting surgery.
To do this, the Trust adopted a range of actions including:
- using data to develop and implement tools to identify patients with a learning disability, understand their experiences and clinical need, and monitor impact of any waiting time. The tools the Trust used included:
- scrutinising information on readmissions, length of hospital stay and mortality for people with a learning disability. This enabled the Trust to target any actions – including prioritising people with a learning disability who were waiting for surgery
- a flagging system within patient records
- a learning disabilities data dashboard
- a data model offering comparisons against the general population
- running a ‘deep dive’ into patient journeys
- auditing the reasonable adjustments made by the Trust, cancer data and missed appointments.
A consultant nurse for learning disabilities leads the work in the Trust. The Trust has also recruited a health inequalities project manager for learning disabilities. The team meets monthly to monitor the waiting lists to ensure people with a learning disability continue to be prioritised within 18 weeks – addressing LeDeR reports which have highlighted that a third of deaths of people with a learning disability were from treatable medical causes. The Trust has also analysed their waiting list data by deprivation and ethnicity; working to narrow any gaps.
Improving reasonable adjustment services in Wolverhampton
In autumn 2022 nurses in the Learning Disability and Autism Team at The Royal Wolverhampton NHS Trust launched a service improvement programme (SIP) to improve the experiences of people with a learning disability attending the hospital.
Patients on a GP learning disability register have a learning disability ‘flag’ on their electronic patient record at the hospital. Flagged patients who have an upcoming outpatient appointment will then receive a phone call from a member of staff at one of the 12 clinics across the Trust that they are due to attend, e.g. fracture clinic, urology, ophthalmology. The patient or their family/carers are asked what, if any, reasonable adjustments are needed when they attend the clinic. The phone call also acts as a reminder to the patient that they have an appointment and staff can reassure nervous patients. These simple adjustments have included:
- doing a practice run so patients can see what is involved in their treatment
- enabling anxious patients to go straight into their allocated appointment or come in through the back entrance
- accommodating patients who have a number of carers
- helping patients to understand any proposed treatment.
The nurses have supported patients through surgery, after general anaesthetics, and attended radiotherapy or chemotherapy sessions. One nurse supported a woman with a learning disability through childbirth while the nursing team also supports patients to understand difficult prognoses.
There has been a significant reduction in the number of patients who ‘did not attend’ an appointment – from around 26% of patients with a learning disability flag missing appointments, (over double the number of missed appointments compared to people without a flag), to almost zero.
Reasonable adjustments are documented in the patient’s electronic record. These records can also be used for inpatients with a learning disability and can be built upon over time – for example by adding a patient’s hospital passport with details of their likes and dislikes, or any accessibility issues.
The service improvements are helping over 3000 people on the learning disability register locally and the team are now working to use a similar system of applying reasonable adjustments to over 1000 patients who are identified as being autistic. Patients are experiencing better health outcomes by being able to be seen in a timely manner, appointment slots are not being wasted and patients are having better experiences in their person-centred treatment.
Social prescribing and personal health budgets (PHBs)
The NHS Long Term Plan (2019) included plans to roll out a personalised care model across the country, to expand the choice people have in their mental and physical health care and control over it. One aspect of this model includes a social prescribing offer, which widens and diversifies the range of support available to people. Link workers in PCNs work with people to develop tailored plans and connect them to local groups and support services for both physical and mental health. Social prescribing is also an integral part of the improvements to AHCs for people with a learning disability and autistic people.
Another component of personalised care is personal health budgets. A personal health budget is an amount of money to support a person’s health and wellbeing needs, which is planned and agreed between a patient (or their family/carer), and their local NHS team. It is not using new money, but using money already available for care and support and spending it differently to allow people to receive support that best suits them. It also enables people to make informed choices when their health changes.
Social Prescribing pilot in Luton
A new social prescribing pilot has been devised by Bedfordshire, Luton and Milton Keynes (BLMK) ICS, to explore how social prescribing, following an annual health check (AHC), might help to reduce health inequalities and improve health and wellbeing for someone with a learning disability.
Medics PCN, a network of five GP practices in Luton, is one of the PCNs involved in the pilot. When a person on the learning disability register attends a practice for their AHC they receive a leaflet describing the ‘social prescription’ activities and groups in and around Luton which are available for adults with a learning disability. The PCN is already seeing success with the scheme and to date over 30% of their patients with a learning disability have been referred to the social prescription service and have utilised a personal health budget (PHB) to improve their overall wellbeing.
For example, physical activities include disability football and martial arts; activities to improve mental health include friendship clubs, life skills activities are available around food and nutrition and money management, and independent life skills sessions include visits to libraries, museums, shops and the local area. Attendees also learn about relationships, communication, transport and personal hygiene.
Patients have used their PHB for activities including gym membership. James, an adult with a learning disability, used his PHB with agreement from the PCN to buy his winter walking boots and a coat so he could keep his wellbeing up through his daily activity of walking for health. Lucy, who is also an adult with a learning disability in the PCN described at her health check how she feels low during the winter months. Lucy’s PHB was subsequently used to buy arts, crafts and jigsaws which she has been able to complete at home during the cold weather.
Medics PCN aims to continue the pilot - their social prescriber and care coordinator plan to visit the residential homes for people with a learning disability in their area.
BLMK ICS also funded training in September 2022 for 13 Medics PCN staff, delivered by the MacIntyre Charity, to help them to support patients with a learning disability. The full day training included understanding the principles of person-centred planning, making reasonable adjustments to social prescribing and learning skills to support shared decision making with patients, families and carers.
Medics PCN will continue to offer all patients with a learning disability an appointment with a social prescriber and patients will be supported with an introduction to free activities and groups.


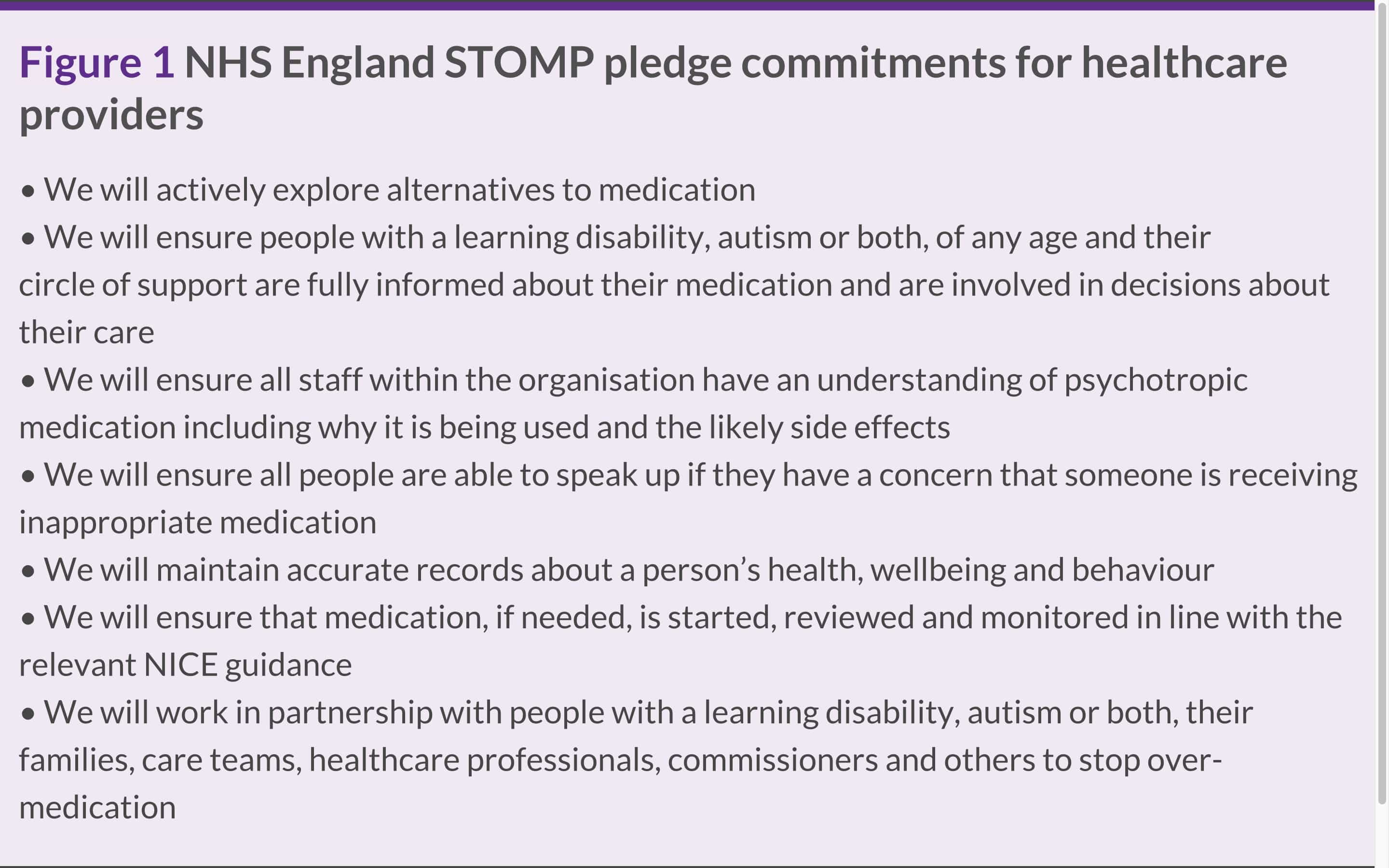
STOMP and STAMP (Medication)
'STOMP’ stands for stopping over-medication of people with a learning disability and autistic people with psychotropic medicines. These are medications which affect how the brain works. ‘STAMP’ supports the treatment and appropriate medication for children and young people.
The STOMP and STAMP programme helps children, young people and adults, with their family, doctor, pharmacist and other organisations involved in their care to consider removing medication, if they no longer feel it is beneficial. It also supports alternatives to medication where appropriate such as, NHS talking therapies, social prescribing and positive behavioural support.
In 2022/23 the STOMP and STAMP programme’s work has included:
Prescribing:
The latest data [27] shows that psychotropic prescribing rates have fallen for people with a learning disability and autistic people, for medications including antipsychotics (often prescribed for behaviour thought to be challenging as well as for mental ill health), benzodiazepines (a type of sedative), and anti-epileptics (where prescribed other than to treat epilepsy). This is welcomed. However, the prescribing rates for anti-depressants have increased year on year for the last five years. Data show that people with a learning disability are still 16 times more likely to be prescribed anti-psychotic medication, and autistic people are seven times more likely to be prescribed anti-psychotics than the general population.
Training:
- We launched six new training modules with the educational platform MindEd - for self-advocates, health and social care staff and families/carers. The 30-minute modules explain the principles of STOMP, and how medicines are prescribed, reviewed, monitored and removed. The modules are available on the Health Education England website and by summer 2023 the six sessions had more than 7000 launches – a significant uplift since spring, reflecting the renewed prioritisation for STOMP and STAMP. The four top job roles accessing the online training were student nurses, nurses, doctors and pharmacists.
- We launched four new training modules in summer 2023 for specialist teams – i.e. psychiatrists, psychologists, pharmacists, specialist nurses, mental health trusts, community teams and staff in social care. These are being promoted extensively across health and social care networks.
Community of practice pilot:
- The Pharmacy Integration Programme funded a pilot led by the NHS England STOMP and STAMP team to look at the level of confidence among Primary Care Network (PCN) pharmacists (who sit within GP practices) to complete structured medication reviews (SMRs) for people with a learning disability and autistic people. Most regions in NHS England took part.
- The pilot included educational webinars and support from experts, and surveys to capture the progress of the 145 pharmacists who carried out SMRs for people with a learning disability and autistic people. More than 100 people whose medication was reviewed are now on a dose reduction plan and 41 people have had their psychotropic medicine stopped.
Raising awareness of STOMP and STAMP:
- In January 2023 the STOMP and STAMP programme hosted an event for people with a learning disability and autistic people. This was led by Carl Shaw, a learning disability and autism advisor for NHS England. The session focused on helping people to communicate how they feel about their medication in an accessible format, for example, where they are non-verbal or might use Makaton, drama or art. The session also advised people on how to get involved in the decision making around their medication, as well as growing confidence to ask about medication and alternatives to medication.
- Delivering several STOMP webinars for pharmacists and pharmacy leaders in the newly formed ICBs, focusing on:
- how to improve communications with people with a learning disability
- workshops sharing the alternatives to medication
- sharing the learning and successes of the PCN pilot (above).
- ran ‘deep dive’ exercises (discussion groups) - for a range of health and care professionals working in specialist teams (learning disability in-patient and community based teams) social care professionals, people with a learning disability and autistic people and family carers to gain insights into the STOMP and STAMP programme in practice. This has highlighted the need for clearer standards of practice, professional accountability and improved inclusion of people and their carers in medication related decisions.
London’s STOMP in action
When safe and wellbeing reviews (SWR) of all people with a learning disability and autistic people who were being cared for in a mental health inpatient setting were completed in January 2022 the oversight review panel in South West London ICB included an Advanced Specialist Pharmacist (in Learning Disability). It was established that at least nine of the 35 reviewed patients had been prescribed psychotropic medicines without a clear documented mental health diagnosis – a key consideration for STOMP. As a result, changes to local quality monitoring were made to increase scrutiny in the use of psychotropic medicines.
South West London trialled specialist pharmacist input in CTRs/CETRs early on and over the last two years the pharmacist has advised on over 30 CTRs/CETRs for people within the South West London ICS footprint, reviewing - and where appropriate - reducing high doses of psychotropic medication and ensuring all the required monitoring is completed. The SWR panel recommended increased involvement of a specialist pharmacist in CTRs/CETRs, especially where people are prescribed complex medication regimes.
The Advanced Specialist Pharmacist has provided training to upskill more than 60 pharmacists in PCNs in South West London since July 2021 to do structured medication reviews with people. This has increased capacity and built confidence among the PCN pharmacists. The specialist pharmacist is also a member of the local LeDeR governance group and has promptly embedded any learning from LeDeR into the training. She now plans to deliver the same training to the pharmacy workforce in all acute trusts across South West London by Summer 2023 to compliment the Oliver McGowan mandatory training on learning disability and autism - with an added emphasis on medicines optimisation.
The wider NHS England London region also recruited a new project manager in early 2023 who will lead on STOMP and STAMP in the region – in the first role of its kind in the country. The role includes oversight of STOMP and STAMP, ensuring each ICS has proper governance in place to challenge inappropriate prescribing and facilitating the sharing of good practice and learning in the region.
-
19 Birmingham and Solihull ICS: Annual LeDeR Report 2021-2022 (Page 20). ↩
-
20 FutureNHS: (Autism Strategy Dashboards) – This is an internal workspace for NHS colleagues. ↩
-
21 Weir, E at al. Increased prevalence of non-communicable physical health conditions among autistic adults. Autism; 9 Sept 2020. ↩
-
22 FutureNHS: (Autism Strategy Dashboards) – This is an internal workspace for NHS colleagues. ↩
-
23 Based on 2022- 2023 data for Sheffield, resulting in an AHC uptake at end of March 2023 of 84.8% (against a 75% target). ↩
-
24 LeDeR Annual Report 2021: King’s College London et al. (Page 26) https://www.kcl.ac.uk/ioppn/assets/fans-dept/leder-main-report-hyperlinked.pdf ↩
-
25 National End of Life Care Intelligence Network (NEoLCIN) (2010) and National Council of Palliative Care and Public Health England (2015). ↩
-
26 Baranek GT, David FJ, Poe MD, Stone WL, Watson LR (2006) Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology and Psychiatry, 47(6), 591-601. And Leekam SR, Nieto C, Libby SJ, et al (2007) Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894–910. ↩
-
27 Health and Care of People with Learning Disabilities Experimental Statistics 2021 to 2022 (December 2022), NHS Digital. ↩